
Textile-based biomaterials, or biotextiles, have the longest history in the field of biomaterials. In ancient China and Egypt as far back as 2000 B.C., natural fibers such as linen, silk, bark, horsehair and dried guts were used as suture materials for wound closure. The introduction of steel wire and synthetic fibers such as polypropylene, nylon and polyester, during and after World War II, brought the first revolution of medical textiles and greatly expanded the chemical composition of textile-based biomaterials beyond natural sources.
Textile structures
Among the natural fibers, silk is the only one that has been successfully adopted in the modern implantable medical textile field. Owing to their precisely controlled manufacturing processes, as well as their uniform and reproducible properties, synthetic fibrous biomaterials have received a great deal of attention from the medical industry, surgeons and researchers. However, basic textile structures such as braided, twisted, knitted, woven and nonwoven have not kept up with the much faster pace of development and advancement of new materials.
The textile structure advancement that has been most biomedically significant is electrospun fibrous membranes, particularly nanofiber-sized membranes used as scaffolds for tissue engineering and regeneration. Most research and development activities have focused on new materials, particularly absorbable or biodegradable materials, instead of on creating a new textile structure.
Distinctive and diverse
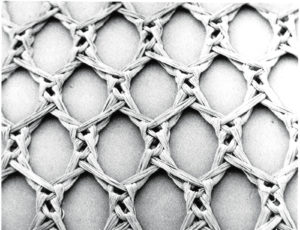
textile-based biomaterials with various chemical, physical, mechanical, textile structural and biological properties for their specific clinical applications. Mersilene mesh, often used. in hernia repair, is made from knitted poly(ethylene terephthalate) fiber.
Today, surgeons can choose among many textile-based biomaterials with various chemical, physical, mechanical, textile structural and biological properties for their specific clinical applications. Textile-based biomaterials are different from other biomaterials largely in their physical form and anisotropic mechanical behavior. They are the only class of polymeric biomaterials outside hydrogels that could have a wide range of three-dimensional porous structures. The most widely used textile structures used as biomaterials are woven, knitted, nonwoven and braided. Within each of these four classes of textile structure, there are many other variations, such as weft knit and warp knit.
These structural features and the wide range of structural possibilities and mechanical strength orientation provide the unique advantages for their numerous applications in biomedical fields, such as in heart valve devices, vascular grafts, tissue engineering scaffolds, surgical meshes, wound closure, tendon or ligament prostheses and in a variety of surgical implants.
Implantable medical textiles are indispensable for the repair and reconstruction of the human body, particularly in the areas of wound closure, cardiovascular implants and surgical meshes for body wall repair. They require great technical sophistication because of the safety, biological complexity and challenges of the human body, in addition to regulatory hurdles.
Among these three areas of application, the textile biomaterials for wound closure are especially important, not only because they are used in virtually every surgery, but also because these textile-based materials have a historical tie to traditional textile materials—such as silk, polyester, nylon and polypropylene—used for nonmedical purposes.
Suture materials
Wound closure biomaterials are generally divided into three major categories: suture materials, tissue adhesives and staplers. Only the suture materials are in textile form. They also have the largest market share, receive the most research and development attention, and are the most widely used in wound closure for surgery. The world market size of sutures is expected to reach about $4.40 billion by 2021, a 27 percent increase from $3.46 billion in 2016.
Suture materials are commonly classified by absorbability or biodegradability in biological tissues, size, physical configuration (monofilament vs. multifilament, braided vs. twisted), and type of coating materials used. These classifications facilitate proper handling during wound closure and provide additional functionality such as antimicrobial properties. Coating materials mainly apply to multifilament braided suture fibers. These facilitate an easier passage through tissues with less resistance during wound closure, and also reduce wound infection since suture fibers, particularly those multifilament braids, are a source where bacteria can hide.
Suture materials have vast differences in chemistry, physical/mechanical properties and biological characteristics. Most of the common fibers used for conventional textiles and apparel purposes (nylon 6,6 or 6, aromatic polyester, polypropylene, GORE-TEX® or silk) have been adopted for non-absorbable suture materials. Synthetic absorbable suture fibers, however, have been made from a new family of aliphatic polyesters developed in the early 1970s. If a suture is absorbable, its tensile strength loss must match the healing rate of the tissues to be closed, and the degradation products must be biocompatible and be metabolized by normal body metabolic mechanisms.
Cardiovascular devices
Vascular diseases frequently result in either the loss of lives or limbs, so the development of textile-based vascular grafts has been one of the most important biomedical advancements. There has been significant progress, allowing medical professionals to reconstruct obstructed or injured blood vessels with remarkable success. The vascular graft market had a value of $2.48 billion in 2016, and it is projected to reach $3.80 billion by 2022.
Serious problems remain unsolved, however, such as full-wall healing. While homografts are still considered to be the preferred arterial replacement for small-diameter vessels (below the knee), they are used in limited quantity and are insufficient to meet the increasing needs for vascular replacement, due mainly to an inadequate supply, nonuniform properties and difficulty in preparation.
The two most important fibrous polymers used for making vascular fabrics are poly(ethylene terephthalate), which has the largest market share, and expanded poly(tetrafluoroethylene). In addition, the use of polyurethane-based elastomeric fibers like spandex has been tried for improving the compliance of vascular grafts. The inherent porous nature of textile materials provides the space fibrous connective tissue needs to grow into in order to achieve full-wall healing.
Currently, there are three basic textile structures—all different from each other in porosity, mechanical and biological properties—for vascular fabrics: woven, knitted and nonwoven. All woven and knitted vascular fabrics are made from poly(ethylene terephthalate), while the nonwoven vascular fabrics are made from expanded poly(tetrafluoroethylene), the same polymer used in the non-absorbable GORE-TEX suture.
Beyond the traditional all-textile-based vascular grafts, a relatively new vascular graft design became available as stent grafts that merge newer stent technology with traditional textiles. The main advantage of stent grafts, usually used to treat aneurysms, is they require less invasive surgical procedures and can be delivered via a catheter.
The most important criteria in designing vascular fabrics are porosity and non-thrombogenic surface. These are closely related because vascular fabrics require porous space for tissue ingrowth, which would ultimately lead to the formation of non-thrombogenic surfaces, which is one of the most important goals in the repair of damaged or diseased vascular systems. Incomplete healing imposes the continued risk of thrombotic occlusion, particularly in medium- and small-caliber blood vessels.
Because all of the existing commercial vascular grafts are constructed from a single type of non-absorbable fiber, poly(ethylene terephthalate) or poly(tetrafluoroethylene), their porosity is relatively constant and does not change with time. It is impossible to vary the porosity of these single-component fabrics so that they would be both very tight during implantation (i.e., low bleeding porosity) to prevent the occurrence of blood leakage, and very porous during healing (i.e., high healing porosity) to promote fibrous tissue ingrowth for a full-wall healing.
There are several approaches to try to design ideal vascular fabrics that would meet these two most important porosity criteria. Among them, the use of absorbable fibers as the sole component or as one of two components of a fabric, and the theoretical prediction of the porosity of a fabric based on some mathematical formula, are quite intriguing and appear to be promising for the design of the next generation of vascular fabrics.
Surgical mesh fabrics
Another common implantable medical textile product that has a long history of saving human lives is surgical mesh for body wall repair. Defects of the body’s tissues are the direct result of the radical resection of a cancer tumor, congenital lesions, infection and subsequent necrosis and debridement, violent crimes, accidents or large hernias.
For large defects such as hernias that lack adequate tissue to permit primary repair, it is desirable to use materials of either a synthetic or a natural origin to reinforce tenuous aponeurotic closures and/or to bridge large defects in the abdominal or chest wall. A wide variety of biological and synthetic textile materials have been used to repair a defective body wall.
Research continues in biomedical textile materials to improve the performance of these materials that are critical in today’s practice of medicine.
C. C. Chu, Ph.D., is the Rebecca Q. Morgan ’60 endowed chair professor, Department of Fiber
Science and Apparel Design and Biomedical Engineering Field, Cornell University, Ithaca, N.Y. (http://chu.human.cornell.edu/).
Readers interested in an in-depth reading of this subject are invited to contact Janet Preus, senior editor, Advanced Textiles Source, (jlpreus@ifai.com), to obtain a list of reference materials provided by Dr. Chu.
 TEXTILES.ORG
TEXTILES.ORG


